Arthroscopy – Knee
ACL TEAR
1. What is an ACL tear?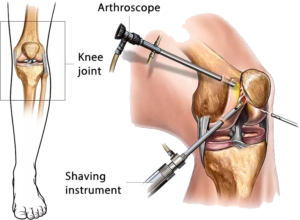
Ans: ACL is thick with fibro-collagenous tissue connecting the lower end of the thigh bone and the upper end of the leg bone. It is one of the important ligaments inside our knee joint which gives stability. It is the most common ligament injury in sports or RTA in our region.
2. How does an ACL tear?
Ans: It is the most common ligament injury in the knee. Any contact sports involving twisting of the knee joint can cause an ACL tear. Eg. Football, volleyball, rugby, etc.
3. What is the treatment?
Ans: Acute injury is treated is conservative with Brace and analgesics. After 3-6 weeks of review if there is instability, then they need to undergo ACL reconstruction.
4. How is ACL reconstruction done?
Ans: ACL is reconstructed with a graft which is a PTB (Patellar tendon-bone) or Hamstrings ( semi tendinosis or gracilis ) muscle This graft is fixed by various methods like titanium screws, bioabsorbable screws, endo button, and tight rope.
5. What is your preferred technique And how is it different?
Ans: We do an “all-inside ACL reconstruction with graft link tightrope technique”. The advantages of this technique are that it is very strong, a single semitendinosus graft is enough, and NO screw or threads prominence over the tibial insertion site. Leg bone outer side is not tunneled, so less painful and hence early recovery. Only very few surgeons are doing this all-in technique.
POSTERIOR CRUCIATE LIGAMENT(PCL)
1. What is PCL?
Ans: Posterior Cruciate ligament(PCL) is another ligament inside the knee joint which is stronger than the ACL ligament and is less often torn. It is a very important structure for knee stability. It has to be reconstructed if it is torn completely
2. How is PCL tear treated?
Ans: A completely torn PCL is reconstructed with a hamstring graft done arthroscopically. PCL is reconstructed in a similar fashion to ACL with special instruments but needs a lengthier graft.
MENISCUS
1. What is a meniscus?
Ans: Meniscus is a thick fibrocartilaginous tissue inside the knee joint. There are two menisci in the knee joint. They function as shock absorbers and get smooth knee movements in the knee joint.
2. What happens if one gets a meniscal tear?
Ans: Meniscal tear is the most common injury to the knee. A tear in the meniscus presents as pain in the knee joint on weight-bearing, locking of the knee joint while walking, or simply pain with swelling.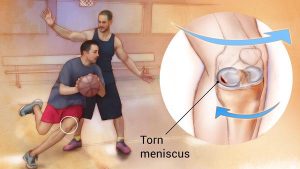
3. What is the treatment for Meniscal Tear?
Ans: Meniscus is a semi-circular structure with a broad outer edge and thin inner edge. Tears towards the outer edge have a good blood supply and heal well with repair and tears towards the inner edge and irregular tears are not repairable and so they undergo partial meniscectomy i.e torn part of the meniscus is removed and the remaining part is trimmed smoothly to prevent a further tear.
4. How is the meniscus repaired?
Ans: There are various kinds of techniques available and are dependent on the area of a tear over the meniscus. The repair technique is based on the tear pattern.
5. Do I get arthritis if my meniscus is removed?
Ans: Arthritis can occur after 10-15 years if the meniscus is removed completely, but nowadays meniscus is preserved to the maximum with the latest techniques of repair or partial meniscectomy to prevent secondary arthritis.
